Executive Summary (TL;DR)
U.S. hospitals spend $19.7 billion a year on administrative appeals of denied claims (OIG 2023), while roughly 15 % of all initial claims are rejected (STAT 2024). Those denials jeopardise ≈ 3.3 % of net patient revenue (≈ $4.9 million per 250-bed facility).
The AI Billing-Code Optimizer plugs into the Electronic Health Record (EHR), reads clinical notes in real time, and surfaces the most accurate Current Procedural Terminology (CPT) and International Classification of Diseases (ICD) codes. By checking payer rules up-front, it prevents avoidable denials. Early pilots show a 3–5 % reimbursement lift and 25–30 % cut in manual coding hours, delivering ROI within 6–9 months.
Problem / Opportunity
- $19.7 B annual administrative spend on denial appeals (OIG).
- 15 % first-pass denial rate; payer mix skews: Medicare Fee-For-Service ≈ 21 %, commercial ≈ 11 % (CMS CERT 2024).
- 78 044 ICD-10-CM diagnosis codes + 11 163 CPT procedure codes (FY 2024) overwhelm coders.
- 86 % of denials potentially avoidable (Change Healthcare 2024).
- National medical-coder vacancy ≈ 30 %, cutting output from ≈ 140 charts/day to 105 (25 % loss, AMA 2023).
Solution Overview
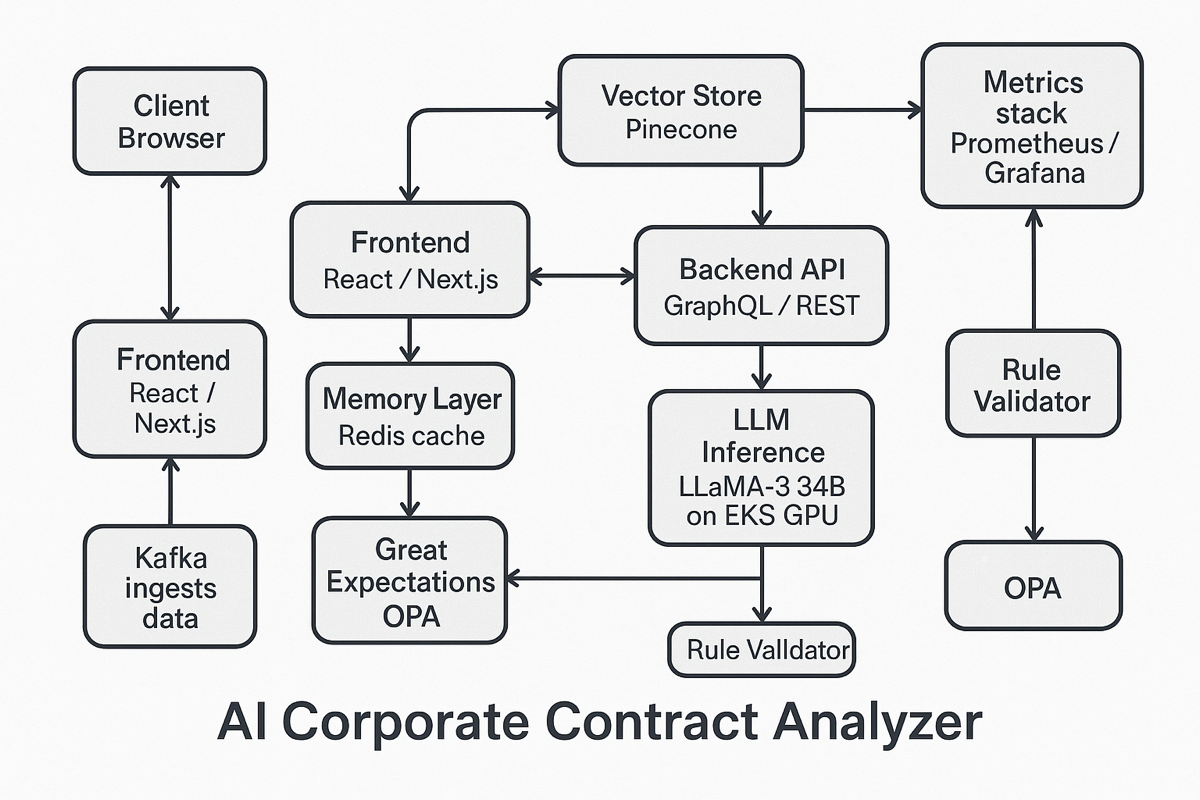
- Context-aware NLP pipeline (note-parser + code-ranking model) analyses notes, labs, and dictations to surface the top-3 compliant codes with confidence scores.
- Rules + Retrieval-Augmented Generation (RAG) engine cross-checks Centers for Medicare & Medicaid Services (CMS) guidance and payer bulletins in real time, flagging high-risk modifiers.
- Interactive coder cockpit displays rationale and a full audit trail; one-click accept or override keeps humans in the loop.
- FHIR and HL7 APIs embed in Epic, Cerner, and Athena with Single Sign-On (SSO).
- Continuous learning loop retrains models on payer adjudication feedback to keep accuracy climbing.
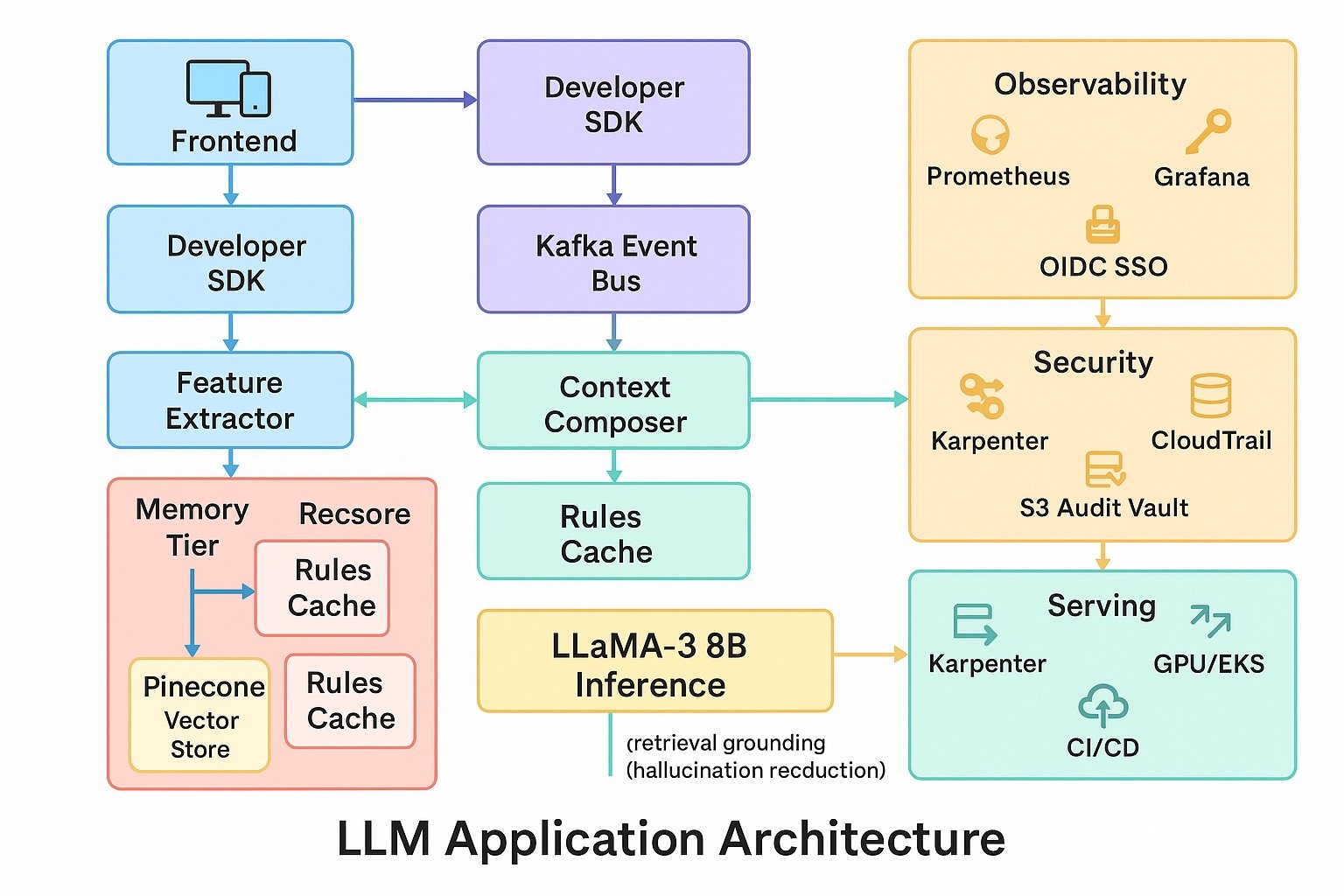
Technical Approach
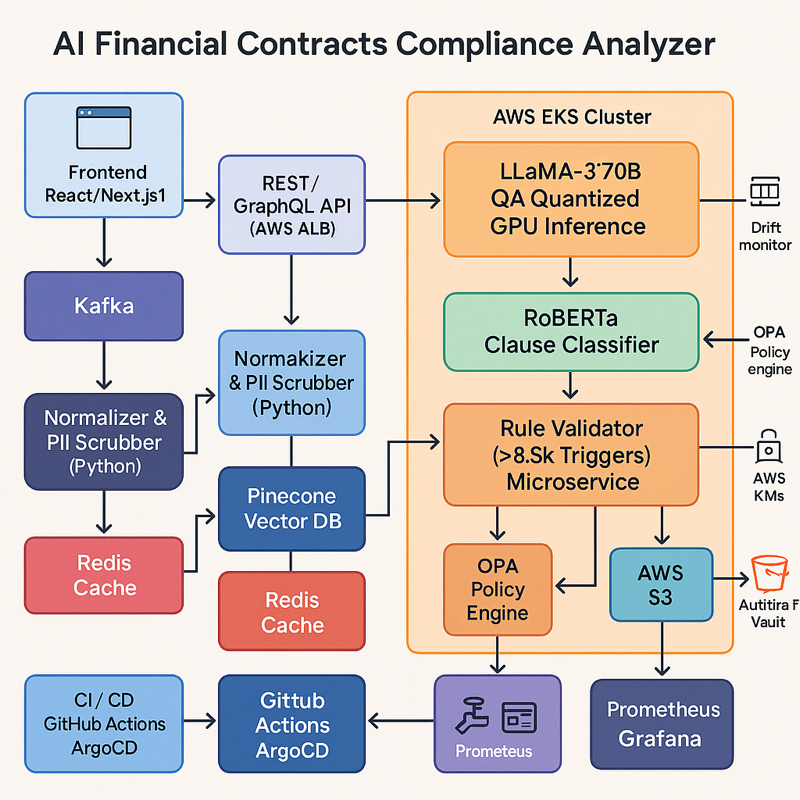
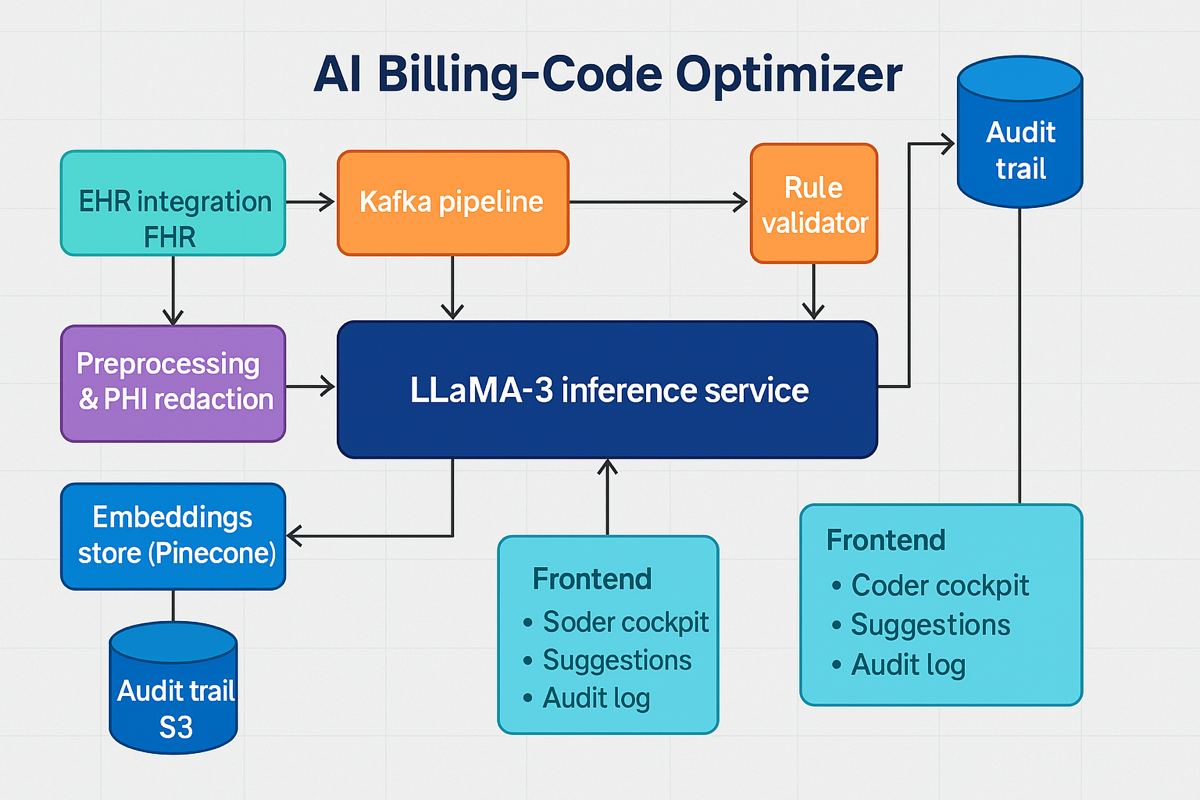
- Model stack.Fine-tuned LLaMA-3 34B-Q4_K_M (int-4) with domain adapters. Secondary XGBoost classifier routes out-of-distribution notes for human review. Rule-based validator (> 3000 payer-specific modifiers and Local Coverage Determinations) ensures compliance.
- Knowledge & retrieval. Hybrid vector + keyword search (Pinecone) indexing CMS transmittals, quarterly payer bulletins, and American Hospital Association (AHA) Coding Clinic articles. CPT/ICD license source (AMA & CMS)Embeddings generated with the open-source BGE-Large model (Llama-compatible). LangChain orchestrates retrieval and prompt assembly.
- Data pipeline. Real-time ingestion of HL7 ORU^R01 and FHIR Encounter resources. Apache Kafka streams data through preprocessing PHI redaction step (spaCy + Philter) → embedding → inference. Great Expectations enforces data-quality contracts and blocks Protected Health Information (PHI) leakage.
- Serving & infrastructure. GPU-backed Amazon Web Services Elastic Kubernetes Service (AWS EKS) auto-scales LLaMA pods; Weights & Biases tracks model drift. Deployed on AWS GovCloud with Key Management Service (KMS) encryption, Virtual Private Cloud (VPC) isolation, and System and Organization Controls (SOC 2) compliance. Blue-green Continuous Integration / Continuous Deployment (CI/CD) via GitHub Actions and ArgoCD.
- Security & audit. OAuth 2.0 / OpenID Connect for SSO; AWS CloudTrail logs every inference; immutable Amazon S3 bucket stores audit events for seven years; Open Policy Agent (OPA) enforces runtime policies.
- Front-end & UX. React/Next.js with Tailwind UI. WebSocket stream delivers sub-second suggestions. Role-based views for coders, auditors, and revenue-cycle managers; Figma design system meets Web Content Accessibility Guidelines (WCAG) 2.1 AA.
- Observability. Prometheus metrics and Grafana dashboards (latency, throughput, GPU utilisation). Sentry captures front-end exceptions; PagerDuty escalates Service Level Agreement (SLA) breaches.
Business Metrics (Targets)
| KPI | Target | Notes |
| Reimbursement lift | +3–5 % | Conservative vs publicly reported highs |
| Denial-rate reduction | ≥ 30 % | Leaves cushion below bold 40 % claims |
| Coder adoption | 50 % Daily Active Users (DAU) by Month 3 | Reflects staged roll-out |
| Customer satisfaction | Customer Satisfaction (CSAT) ≥ 4.5 / 5 | Survey of revenue-cycle managers |
Product Metrics (Targets)
- F1 ≥ 0.92 on top-3 prediction
- Median latency ≤ 1 s
- System uptime ≥ 99.7 %
- Audit-flag precision ≥ 0.90
Expected Impact
A 250-bed hospital faces ≈ $5.3 million/year in appeals overhead (19.7 B ÷ 919 k beds × 250).
By eliminating avoidable denials and lifting reimbursements 3–5 % on the $4.9 M at-risk baseline, the optimizer recaptures $1.0–$1.5 M net patient revenue. Cutting coder effort 25 % releases ≈ 1.9 FTE, while faster first-pass approvals accelerate cash-flow by 10–14 days. Combined, these effects shave >$5 M in administrative drag and revenue leakage, funding the system’s payback inside a fiscal year.
Reference URLs
- Hospital Appeals Cost Burden — U.S. Office of Inspector General
https://oig.hhs.gov/reports-and-publications/workplan-item/contract-appeals-costs - Insurance Claim Denials Compromise Patient Care — STAT News
https://www.statnews.com/2024/05/01/insurance-claim-denials-compromise-patient-care-provider-bottom-lines/ - CERT Improper Payment Rate Supplemental Data 2024 — Centers for Medicare & Medicaid Services
https://www.cms.gov/research-statistics-data-and-systems/monitoring-programs/medicare-fee-for-service-compliance-programs/cert - 86 % of Denials Are Potentially Avoidable — Becker’s Hospital Review
https://www.beckershospitalreview.com/finance/86-of-denials-are-potentially-avoidable-strategies-to-better-prevent-manage-denials/ - FY 2024 ICD-10-CM Code Updates — MedLearn Media
https://medlearn.com/fy-2024-icd-10-cm-code-updates-key-changes-and-highlights/ - CPT® 2024 Code Set — American Medical Association https://www.ama-assn.org/practice-management/cpt/349-ways-cpt-codes-set-prepares-physicians-practicing-2024
- Medical-Coder Shortage and Productivity Impact — AMA Leadership Viewpoint 2023
https://www.ama-assn.org/about/leadership/addressing-another-health-care-shortage-medical-coders
Denials Jeopardise 3.3 % Net Revenue — Healthcare Dive https://www.healthcaredive.com/news/report-262b-in-healthcare-claims-initially-denied-last-year/445758/